A reasearch team from the Medical University of Vienna, the University Medical Center Hamburg-Eppendorf and the Swiss Federal Institute of Technology Zurich (ETH Zurich) have developed a miniature blood pump to treat children with congenital heart defects. This new miniature pump actively transports blood from the body’s veins to the lungs, thus functionally replacing the missing right ventricle. If approved for human use, the pump will save many lives.
Marcus Granegger
17 September 2025
French version | German version
Around 10 percent of all children with congenital heart defects are born with only one functioning ventricle. This rare but serious malformation is known as univentricular cardiac physiology. Affected patients require highly complex heart surgery at an early age in order to survive.
For decades, the Fontan procedure has been considered the standard treatment. In this procedure, the large vena cavae—the superior vena cava (SVC) and inferior vena cava (IVC)—are connected directly to the two pulmonary arteries in several surgical steps. The only functioning ventricle must then pump blood through the body’s circulatory system on its own. The blood flows passively into the lungs without the support of a second ventricle.
Although this method is life-saving, it causes significant long-term problems. The absence of the subpulmonary ventricle leads to unphysiological hemodynamic conditions: pressure in the veins rises, causing venous congestion and fluid retention. In the long term, this can lead to serious complications—from liver disease and cardiac arrhythmia to complete circulatory failure.


For patients with a failing Fontan circulation, a heart transplant is currently the only option. However, donor organs are rare, and the complex anatomy of these patients makes the procedure even more difficult. The reality is that many children and adolescents with Fontan circulation die before a suitable donor heart becomes available. In addition, experts predict that the number of Fontan patients will double in the next 20 years.
A technical solution to an unsolved medical problem
Against this backdrop, an interdisciplinary research team is working on a completely new treatment option: a miniaturized mechanical blood pump that can take over the function of the missing subpulmonary ventricle.
The project is a collaboration between the Medical University of Vienna (University Clinic for Cardiac and Thoracic Aortic Surgery), the University Medical Center Hamburg-Eppendorf (UKE), and the Swiss Federal Institute of Technology Zurich (ETH Zurich).
Dr. Marcus Granegger (MedUni Vienna) is responsible for the technical management, while Prof. Daniel Zimpfer (MedUni Vienna) and Prof. Michael Hübler (UKE Hamburg) are responsible for the medical management. Together with engineers and cardiac surgeons, they have developed a rotodynamic miniature pump with two inlets and one outlet.
This concept is unique: the inlets are connected to the superior and inferior vena cava, and the outlet to the pulmonary artery. The pump actively transports blood from the body’s veins to the lungs, thus functionally replacing the missing right ventricle.
Technological basis and specific challenges
The system is based on technologies that are already being used successfully in conventional cardiac support systems for adults with heart failure. However, two key adjustments were necessary for use in Fontan patients:
- Miniaturization – Children’s hearts and blood vessels are significantly smaller, which requires a drastic reduction in pump size.
- Special flow control – Unlike conventional pumps, the system must accommodate two separate blood flows (from the superior and inferior vena cava).
The development therefore required complex flow simulations (CFD), hemocompatible designs, and extensive laboratory testing.
From simulation to successful animal testing
In recent years, the system has undergone extensive preclinical testing. First, the researchers used computers to analyze how the Fontan circulation changes with the support of the pump. The flow in the pump was then examined with regard to blood compatibility – crucial for preventing blood clots or cell damage.
Following successful blood tests in the laboratory, the decisive step was taken: the first implantation in a newly developed animal model at the Center for Biomedical Research at MedUni Vienna (headed by Prof. Bruno Podesser).
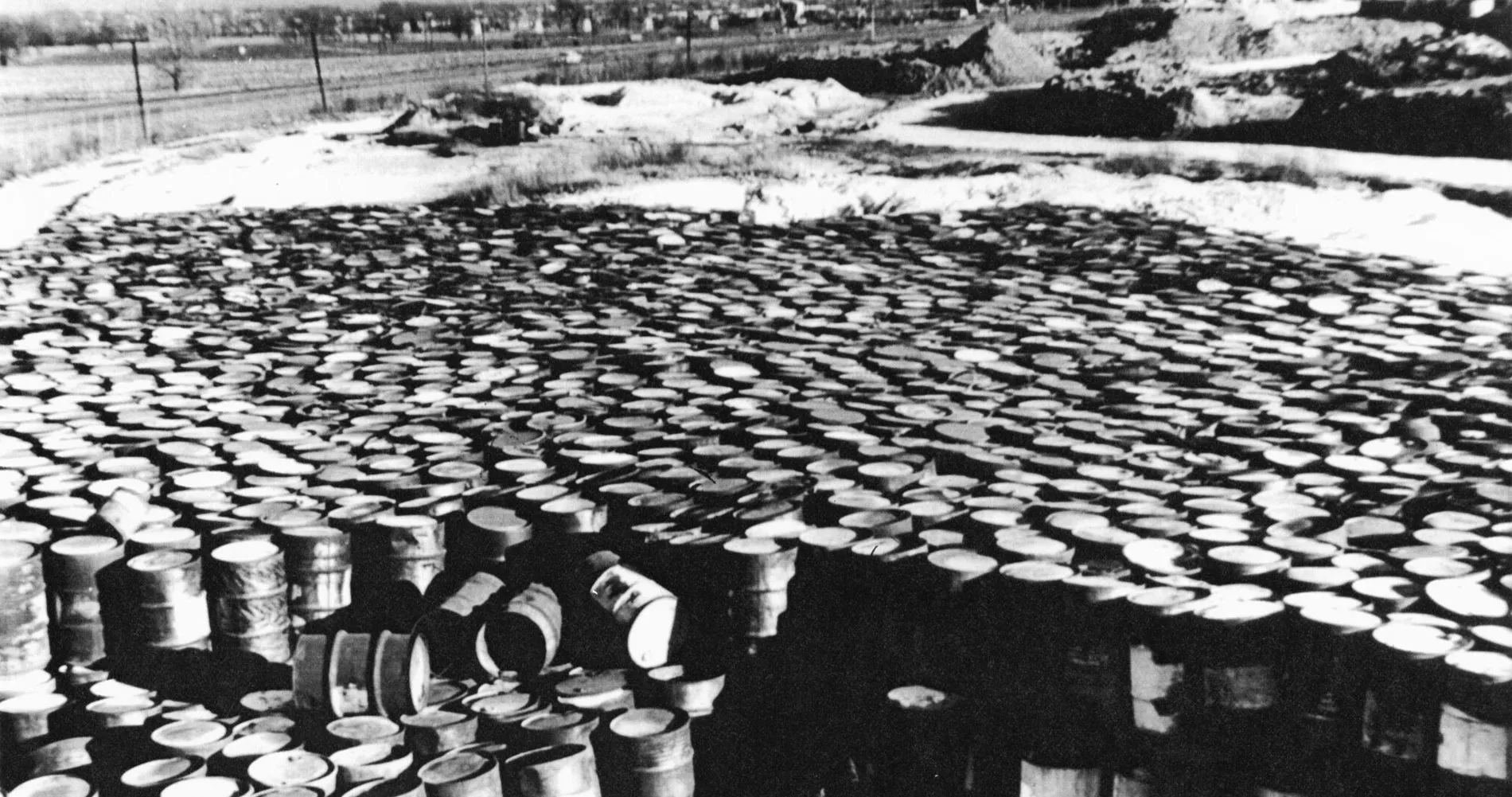
 CPAD control unit
CPAD control unit
The pump was able to completely replace the right side of the heart in sheep – and do so for several hours. Measurements showed that circulation was stabilized, pulmonary blood flow normalized, and there was no significant blood damage.
The next milestone: long-term tests and clinical prospects
The next steps are clear: the team wants to investigate the long-term effects of this support technology in further animal models. The aim is to optimize the pump so that it works reliably over the long term without damaging the blood or surrounding tissue. At the same time, materials, energy supply, and implantation techniques will be further developed.
“Our goal is to offer affected children a therapy that not only ensures their survival, but also enables them to lead active, worthwhile lives – without the constant uncertainty of whether and when a donor heart will be available,” say the researchers.
Hope for a growing group of patients
If the system proves itself in long-term trials, it could become a revolutionary addition to existing Fontan therapy—and open up new prospects for thousands of children worldwide.
Until now, there has been no established alternative to heart transplantation for Fontan patients with circulatory failure. Mechanical support implanted at an early stage could not only prevent the disease from progressing, but also significantly improve quality of life for years to come.
The project is an impressive example of how medical innovation can arise from interdisciplinary collaboration.